Written by Howard Palte, MD, Bascom Palmer Eye Institute (University of Miami)
Today, more than 6 million patients in the USA receive long-term therapy for the prevention of thromboembolism from atrial fibrillation, mechanical heart valves and deep vein thrombosis. Patients undergoing eye surgery are often elderly, have significant comorbidity and receive antiplatelet or anticoagulant therapy. These medications may predispose eye surgery patients to risk of hemorrhagic complications either during the administration of regional anesthesia or intra-orbital intervention. The anesthesia provider is faced with the dilemma of balancing the risk of orbital hemorrhage against the peril of a catastrophic outcome associated with cessation of anticoagulation therapy. In this respect, an appreciation of the pharmacology of the newer anticoagulant agents is key in the management of eye surgery patients.
Heparin and Vitamin K Antagonists
Unfractionated heparin and warfarin have been available for more than half a century but impose limitations, such as slow onset of action, interaction with food and drugs, and narrow therapeutic window. Also, Vitamin K antagonists (VKA) have unreliable efficacy and demand routine coagulation monitoring and dose adjustment to maintain the international normalized ration (INR) in the target range. In addition, the slow onset of action means that many patients require perioperative bridging therapy with a rapidly acting agent (e.g. heparin).
Newer Antithrombotic Agents
In addressing these deficiencies, research development has centered on newer oral agents that inhibit two key serine proteases in the coagulation cascade:
1. Thrombin (FIIa)
2. Activated factor X (FXa).
Thrombin (FIIa) plays a central role in coagulation and clot formation by converting fibrinogen to fibrin and feedback activation of factors V, VIII and XI (see Fig. 1).
Factor Xa is a logical target because it is located at the junction of the extrinsic and intrinsic pathways. FXa inhibition attenuates thrombin formation preventing the conversion of fibrinogen to fibrin (see Fig.1).
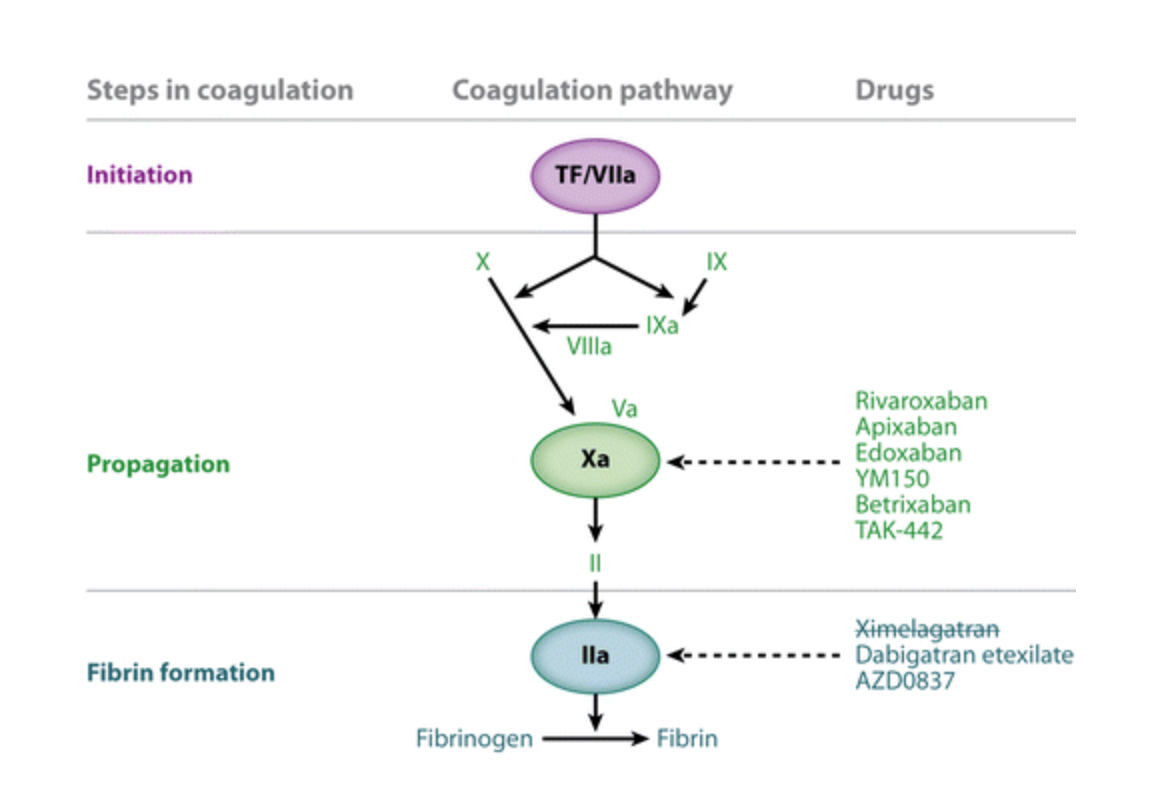
Figure 1. Newer anticoagulants and their targets in the coagulation pathway (adapted from: Erikson et al. Novel Oral Factor Xa and Thrombin Inhibitors)
Advantages of the new oral anticoagulants over VKA include rapid onset of action and few food interactions. However, the greatest clinical benefit of these new oral anticoagulants is their predictable efficacy in attaining a desired level of anticoagulation, thus obviating the need for routine monitoring.
Thrombin (FII) Inhibitor
1. Dabigatran (Pradaxa) - direct thrombin inhibitor, oral bioavailability 6%, dose once or twice daily, half-life (t1/2) 12 hours, no inhibition cytochrome P-450 (CYP).
Factor Xa (FXa) Inhibitors
1. Rivaroxaban (Xarelto) - bioavailability 80%, administered once or twice daily, t1/2 12 hours, potent inhibitor CYP3A4.
2. Apixaban (Eliquis) – bioavailability 66%, dose twice daily, t1/2 12 hours, potent inhibitor CYP3A4.
3. Edoxaban (Lixiana) – bioavailability 50%, dose once daily, t1/2 10 hours, potent inhibitor CYP3A4.
Bleeding Risks of Ophthalmic Surgery During Continuation Antithrombotic Therapy
The predominant concern surrounding continuation of antithrombotic therapy is the risk of hemorrhage with placement of an ophthalmic block or during surgery. Block-induced hemorrhage can have devastating consequences leading to compressive hematoma, retinal ischemia and loss of vision. However, the main risk factor for periorbital hemorrhage is arterial fragility rather than hemostatic disorders. These devastating complications can be minimized by adopting single injection techniques, short needles (<25G and <25 mm), limited depth of needle insertion, minimal angulation, and injection in the vascular-poor infero-temporal quadrant.
Cataract Surgery
In most centers phacoemulsification surgery is performed under either topical anesthesia alone or with intracameral preservative-free supplementation. A meta-analysis of 11 studies found that patients who continued oral anticoagulants had an increased bleeding risk but these were insignificant (subconjunctival) and self-limiting.
Vitreoretinal Surgery
In recent years there have been a number of studies addressing continued antithrombotic therapy in patients undergoing vitreoretinal surgery. An observational study of 822 patients identified five risk factors for bleeding; male sex, smoking history of proliferative diabetic retinopathy, glaucoma and anticoagulant use. Although anticoagulants were associated with increased risk of intraorbital hemorrhage there were no serious sequela, need for re-operation or surgical failures. Posterior segment surgery is commonly performed under regional anesthesia but the incidence of retrobulbar hemorrhage following an ophthalmic block is exceptionally low. There is no evidence-based data to substantiate that regional ophthalmic anesthesia amplifies risk for retrobulbar hemorrhage.
Glaucoma Surgery
Two recent studies reported a higher incidence of hemorrhage during or after cutaneous surgery in patients on antithrombotic therapy but without serious consequence. For oculoplastic procedures, the incidence is also very low; one American survey found an incidence of 1:2000.
Conclusion
There are no randomized controlled trials that directly compare the rate of thromboembolic events associated with anticoagulant discontinuation against periorbital hemorrhage secondary to ongoing therapy. Severe sight-threatening block-related hemorrhagic complications are rare. Therefore routine cataract, glaucoma, vitreoretinal and oculoplastic procedures appear to be safe in patients on antiplatelet and vitamin K antagonists, as long as the INR is within therapeutic range. On balance there is insufficient data to substantiate firm recommendations for the newer antithrombotic agents (rivaroxaban, dabigatran, apixaban) but clinical experience supports continuation of therapy.
Prudence dictates assessment on an individual basis, and on occasion, liaison between the anesthesia provider and cardiologist or neurologist. Ultimately, management decisions in regard to perioperative anticoagulation rely on best clinical judgement.
Suggested Reading:
1. Management of antithrombotic therapies in patients scheduled for eye surgery. Bonhomme et al. European Journal Anaesthesiology. 2013.
2. Novel oral factor Xa and thrombin inhibitors in the management of thromboembolism. Eriksson et al. Annual Review Medicine. 2011.
3. Ophthalmic patients on antithrombotic drugs: a review and guide to perioperative management. K-L Kong et al. British Journal Ophthalmology.2015.
4. Peri-operative management of ophthalmic patients taking antithrombotic therapy. Lip et al. International Journal of Clinical Practice. 2011.
5. The use of perioperative antithrombotics in posterior segment ocular surgery. McClellan et al. American Journal Ophthalmology. 2014.